Introduction: Acute myeloid leukemia (AML) continues to be a major therapeutic challenge. There is an emerging need to develop less toxic and more effective targeted therapies. Natural Killer (NK) cells possess many of the key attributes critical for effective cancer therapies- "born to kill" but without apparent risk of graft versus host disease, cytokine release syndrome, or neurotoxicity. Furthermore, their intrinsic propensity to target myeloid blasts makes them particularly attractive for AML. Despite promising clinical results in blood cancer, the development of NK cell-based therapy remains challenging mostly due to NK cells' short lifespan, inadequate proliferation and lack of specific tumor targeting. Here, we utilized a new approach to arm NK cells for adoptive immunotherapy based on innate cell memory. Chimeric antigen receptors (CARs) significantly enhance anti-tumor specificity and activity of immune effector cells. Our innovative CAR-NK cells target a tumor-specific neoepitope in AML and harness potent function pathways in their design to enhance efficacy and minimize toxicity.
Methods:
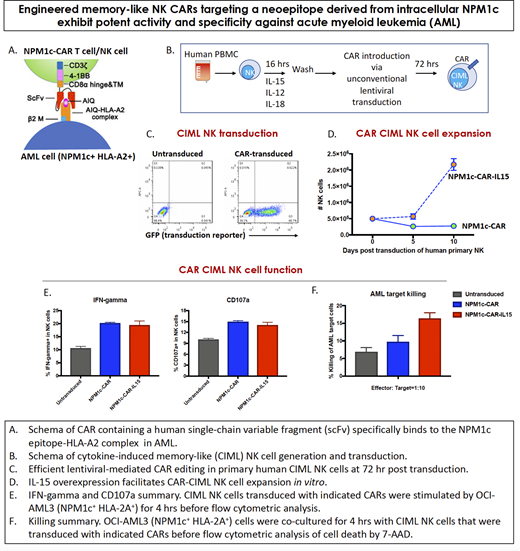
1. Mutated NPM1c as a CAR Target in AML. Most CAR-T cell therapies target tumor-associated antigens (TAAs), which could lead to on-target/off-tumor toxicity as well as tumor resistance. One way to overcome these drawbacks is to target tumor-specific oncogenic driver mutations. The four-nucleotide duplication in nucleophosmin, referred to as NPM1c, is a driver oncogene mutation in about 35% of AML. The mutation creates a neoepitope that is presented by the most common HLA-A2 allele. Using yeast surface display, we have isolated a human single-chain variable fragment (scFv) that specifically binds to the NPM1c epitope-HLA-A2 complex, but not HLA-A2 alone or HLA-A2 loaded with control peptides.
2. Cytokine-Induced Memory-Like (CIML) NK Cells as a CAR Platform. CIML NK cells can provide a unique platform for development of NK cell CARs based on the favorable safety profile, increased proliferation, prolonged persistence and enhanced anti-leukemia function that we have observed in pre-clinical models (Romee et al, Blood 2012) and in patients (Romee et al, Science Trans Med 2016) treated with un-modified CIML NK cells.
3. Efficient Gene Editing in Primary NK Cells. We have overcome the transduction block in primary human and mouse NK cells by utilizing an unconventional pseudotyped lentivirus based on a unique protein with high expression on CIML NK cells.
Results:
1. Engineered CAR-T cells with the isolated scFv exhibit potent cytotoxicity both in vitro and in vivo against NPM1c+HLA-A2+ leukemia cells (OCI-AML3) and primary AML blasts, but not NPM1c-HLA-A2+ leukemia cells (OCI-AML2) or HLA-A2- tumor cells (PC-3).
2. The in vivo anti-leukemia efficacy of anti-NPM1c CAR-T cells was however transient (overall survival extended from 28 to 42 days, median survival extended from 21 to 37 days, compared with the control mice adoptively transferred with untraduced T cells), with unneglectable toxicity.
3. Utilizing an unconventional pseudotyped lentivirus to transduce CIML NK cells from healthy donor blood (n = 5 donors), we have successfully generated anti-NPM1c CAR-NK cells with high transduction efficiency (using MOI = 10: transduction rate mean 48%, range 32% to 65%; compared with 2%, range 0.8% to 4.5% for the conventional approach with VSVG pseudotyped lentivirus).
4. Harnessing key cytokine pathways in the CAR design substantially promoted CAR-NK cell survival (indicated by the enhanced cell viability from 29.7% to 75.2%) and proliferation (marked by the increased levels of ki-67 from 60.2% to 94.5%).
5. Anti-NPM1c CAR significantly promoted anti-tumor function (represented by CD107a, IFN-gamma) and tumor-specific killing (measured by annexin V and 7-AAD) of CIML NK cells against AML with NPM1c oncogene (OCI-AML3).
6. Dual-armed CIML NK cells with CAR and cytokine signaling exhibited optimal specificity and sustainability against AML targets.
Conclusion: These results demonstrate that the innovative CAR-CIML NK cells could be developed as an efficient cellular immunotherapy for treating NPM1c+HLA-A2+ AML with potentially reduced on-target/off-tumor toxicity and tumor resistance. Our study should drive novel conception and design of CAR-NK cell therapies against myeloid malignancies in the clinic.
Ritz:Rheos Medicines: Consultancy; LifeVault Bio: Consultancy; Infinity Pharmaceuticals: Consultancy; Falcon Therapeutics: Consultancy; Avrobio: Consultancy; Kite Pharma: Research Funding; Equillium: Research Funding; Amgen: Research Funding; Talaris Therapeutics: Consultancy; TScan Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.